Herniated disc
Prolapse and degeneration of the disc
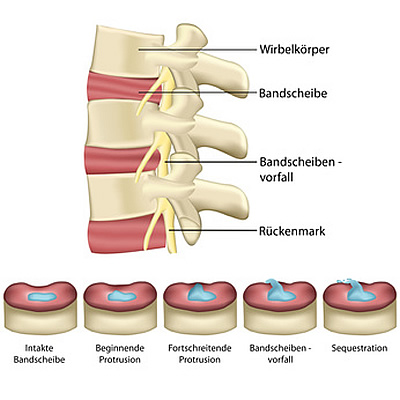
How is the disc constructed?
The intervertebral discs are firmly connected to their adjacent vertebrae and have the task of controlling movement of the vertebrae and bearing the strain on the spine. The intervertebral disc consists of a fibrous ring (annulus fibrosus) made of multiple, intersecting collagen fibres. Together, all of the overlapping fibrous rings form one elastic ring. The core of the disc (nucleus pulposus) consists of gelatinous viscous protein tissue, which when healthy is very strong and stable. In this way, the load of the adjacent vertebrae can be stably transmitted. However, the disc contains no blood vessels (except in the embryonic stage). Nutrients are therefore solely supplied by diffusion. Contrary to standard medical teaching and frequently quoted opinion, Alvin McKenzie (1) and Robert Roaf (2) claim that it is not the discs, but the vertebral bodies themselves which act as the real shock absorbers. Under normal pressure and below critical strain levels, a healthy disc is pushed against the vertebrae, causing the elastic fibre ring to change shape elastically. Under pressure or strain, a healthy vertebra is able to stiffen itself with muscle tension by rapidly absorbing liquid to bear the load (3).
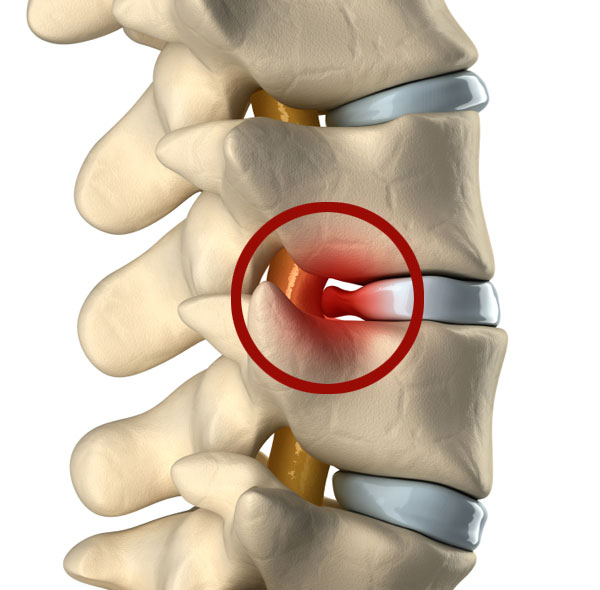
What is a herniated disc?
A herniated disc is a result of degeneration and destruction of the intervertebral disc ring and the nucleus pulposus. Chronic strain, a lack of regenerative capacity of the tissue in old age or even injury to the cartilage plates of the adjacent vertebral bodies lead to a degeneration of the disc tissue. The absence of a blood supply in the disc inevitably leads to a degeneration process. Harmful inflammatory substances ultimately stimulate a cascading breakdown of tissue. This leads to tears in the fibrous ring and under pressure, fragments of the destroyed nucleus pulposus and / or the fiber ring may leak out, presenting a herniated or prolapsed disc. As the fiber ring is thinner at the back, this can compromise the spinal cord and nerve roots (1). The consequences are pain, discomfort or even paralysis in the arms or legs. In a very severe incident, serious complications such as partial or complete paralysis of the spinal cord can occur (paraplegia, causa equina syndrome). (→ see chapter: Therapy )
Animation…
Treatment of herniated disc
As long as there is no nerve interference in the form of paraesthesia or nerve failure in the arms, hands, legs or feet, conservative treatment over several months is recommended. If, however, no permanent improvement of symptoms and freedom from pain is achieved after this period, surgical treatment is usually unavoidable. Indications for surgery (4): – persistent nerve paralysis of the hands or feet – severe, untreatable pain – acute paralysis of bladder and / or rectum.
With surgery on the lumbar spine, the vertebral canal is usually accessed from the rear by a small incision of a few centimeters, made with the aid of the microscope or endoscope. Then the compressing portions of a herniated disc can be removed from the spinal canal to relieve the pressure on the nerve roots. However, the degeneratively destroyed disc can not be reconstructed by this type of treatment. The segment collapse remains, with its described pathology. In medical literature, the rate of recurrence due to new disc herniation, consequent instability damage to the spine, lasting pain and dissatisfying results is rated at up to 33%. [2,4,5,6] In these cases, the implantation of a disc prosthesis is an option to solve this problem, whilst preserving the movement and function of the spine. Disc prolapses on the cervical spine are usually operated on from the front, the whole herniated disc tissue is removed, thereby relieving the spinal canal and nerve roots. Then a ‘placeholder’ (cage) or a disc prosthesis is inserted to stabilise and reconstruct the spine.
Literature
1. McKenzie,A., (2011) Die Grundlagen der bewegungserhaltenden Chirurgie: Lektionen aus der Vergangenheit, S. 2-10, in: Rudolf Bertagnoli et.al. (Hrsg) Bewegungserhaltende Wirbelsäulenchirurgie, Urban&Fischer 2. Roaf,R., (1960) A Study of the Mechanics of Spine Injuries. J. Bone Joint Surg, 42B:810-823 3. Draenert,K., Draenert,Y., (1981) Histomorphology of the Locomotor Apparatus. The Importance of Morphology in Basic Research. Sandorama IV, 9-14 4. Krämer, R., Herdmann,J., Krämer, J. (2004) Mikrochirurgie der Wirbelsäule, Georg Thieme Verlag Stuttgart, New York 5. Fritsch, E. W., Heisel, J., Rupp, S. (1996) The Failed Back Surgery Syndrome: Reasons, Intraoperative Findings, and Long‐Term Results: A Report of 182 Operative Treatments, Spine, Volume 21, Issue 5, Page 626 – 633, Lippincott Williams & Wilkins Inc., Philadelphia 6. Findley.G. et al. (1998) A 10 Year Follow-Up of the Outcome of Lumbar Discectomy, SPINE Volume 23, Number 10, pp 1168 -1171, Lippincott Raven Publishers